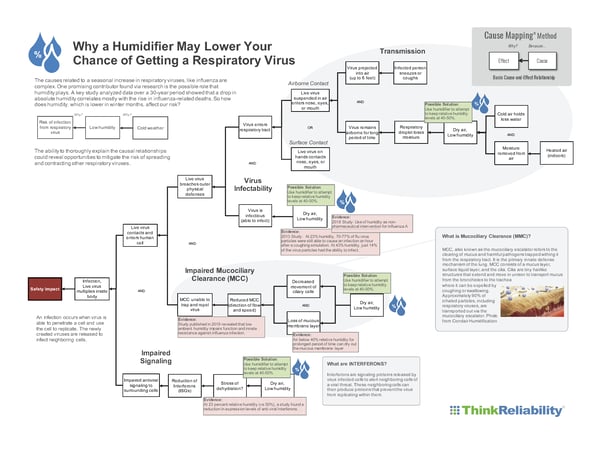
Have you ever wondered why respiratory viruses like colds and influenza are seasonal? There is a complex system of causes that come together to increase our risk during cold, dry winter months. This requires a thorough understanding of the cause-and-effect relationships within being exposed to and contracting a virus. For example, many people recognize cold weather causes increased respiratory infections, but why? How does cold weather result in greater risk of the flu and colds? The ability to more thoroughly explain that causal relationship could reveal opportunities to mitigate the risk of spreading and contracting other respiratory viruses like COVID-19.
The causes related to a seasonal increase in respiratory viruses, like influenza, are complex. One promising contributor, which this blog digs into, is the possible role that humidity plays. A key study that analyzed data over a 30-year period showed that a drop in absolute humidity significantly correlates with the rise in influenza-related deaths. So how does humidity, which is lower in winter months, affect our risk? While there are other causes that contribute to infection, this blog will focus on causally explaining how low humidity has been shown to increase the risk of infection for the influenza virus. Is it possible that the lessons learned could also apply to COVID-19? Let’s take a look.
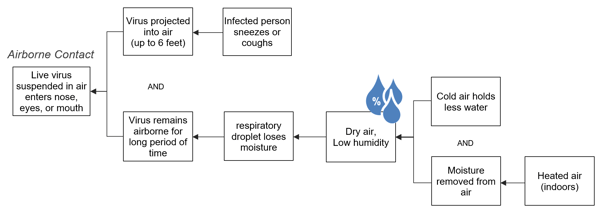
Airborne Transmission: Sneezes, Coughs & Suspended Viral Particles
Most respiratory viruses can be transmitted through the air or through surface contact, but this blog will focus on the airborne contact. When an infected person coughs, sneezes, or even breathes, he or she sheds viral particles attached to respiratory droplets. A sneeze produces 20,000 droplets that can project out up to six feet, potentially putting a significant number of viral particles in the air. (For comparison, a cough produces only a few hundred.) A lot of the larger, heavier droplets will fall to the ground, but smaller droplets can remain suspended in the air, increasing the risk of infection for those in the area. The less humid the air is, the more droplets will remain suspended.
Because this is a complex issue, we’ll use a Cause Map™ diagram to show the cause-and-effect relationships in a visual format. For reference, we start with the effect on the left, and ask Why questions, to begin adding to the chain of events to better understand how a virus enters the respiratory tract. In the below example, we see that a virus enters the respiratory tract through airborne contact or surface contact. As we continue asking Why questions, we see how the airborne contact occurs.
The Cause Map diagram shows that your risk of airborne contact increases the longer a virus can stay suspended in air. Dry air (low relative humidity) can cause the respiratory droplet that virus is attached to lose moisture. Less moisture allows the droplet to remain suspended for a longer period of time, which means it retains a position to infect people longer.
In addition to increasing our risk of airborne contact, humidity can also impact our ability to get infected once the virus is in our body. According to a study published in 2013, at humidity levels of 23 percent, 70 to 77 percent of the flu virus particles were still able to cause an infection an hour after a coughing simulation. But when humidity levels were raised to 43 percent, just 14 percent of the virus particles had the ability to infect.
Most of the flu particles became inactive 15 minutes after they were released into the humid air. That means higher humidity is a way to mitigate the risk of contracting a virus. "The virus just falls apart," at high humidity levels, CDC National Institute for Occupational Safety and Health employee and one of the study’s researchers John Noti said.
In another study, published in 2018, the reduction of absolute humidity was associated with flu outbreaks in temperate climates. For the study, the researchers went into a community preschool and collected samples and objects handled by students (e.g. blocks and markers). They observed a significant reduction in samples with the virus in the classrooms that had more humidity than the control rooms. Their findings suggest that adding humidifiers could be a possible strategy to control flu outbreaks in temperate climates.
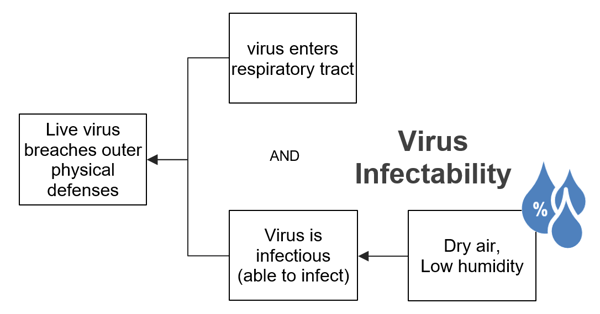
Exactly how humidity affects infectability of the influenza virus is still not understood. But the studies show it is possible that humidity could have the same effect on COVID-19.
Humidity’s Effect on Our Immune Systems
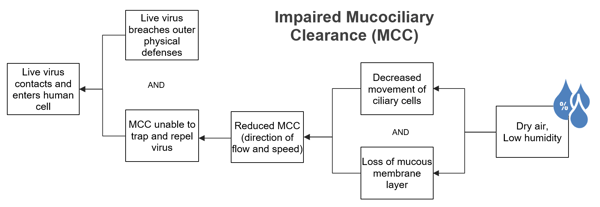
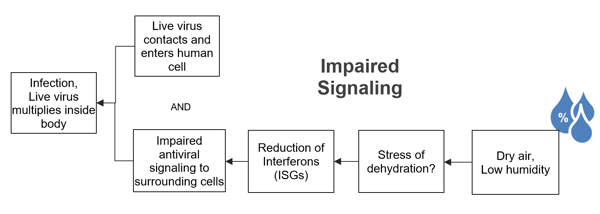
Even if a live virus is able to breach our outer physical defenses, we still have an opportunity to avoid infection and severity, with the help of our immune system. Just last year, Yale researchers published their results from experiments performed on mice that had been genetically modified to resist viral infections as humans do. The researchers found that low humidity hindered the immune response of the animals in three ways: their ability to expel the particles, the ability of airway cells to repair lung damage caused by virus-infected cells and their ability to release signals (interferons) of the viral threat to other cells in the body. These are three layers of protection, or lines of defense, your immune system has against respiratory diseases, and as it turns out, in low humidity environments, they’re less effective.
What’s interesting is that these findings reveal additional causal paths of how humidity may affect risk of infection. For example, in order for the virus to cause infection, it must make contact with a susceptible cell. We all have a mucous barrier in our lungs that traps and works to remove harmful pathogens. Lower humidity can decrease this mucous membrane layer—reducing its movement and attempts to expel those pathogens.
This study also revealed the affect of low humidity on the mice’s ability to keep the virus from multiplying. When a virus infects a cell, the infected cell can release a signal to other neighboring cells, letting them know there is a viral threat to fight. Low humidity was shown to impair these signaling proteins, known as interferons.
Humidity Implications for COVID-19
In an article published by AccuWeather just last week, a team of researchers in China that has been conducting a study on COVID-19 found that high temperatures and high relative humidity may significantly reduce the transmission of this fatal virus. Keep in mind, this is an early study conducted over a limited period of time, but it’s another group of researchers who are suggesting humidity may play a larger role in our infectability than many of us previously realized. Of course, we can’t control the humidity of the regions we live in and we should all be limiting our travel per CDC and governmental guidelines, but many of us, particularly in lower humidity areas may want to consider adding a humidifier to our homes.
With this additional evidence collected from scientific journal articles, we’re able to further expand the Cause Map diagram to include these causal relationships. Doing so, we find the opportunity to reduce the risk of infection on four causes by increasing the relative humidity of our environment to least 40 percent. Download a PDF of the Cause Map diagram by clicking the thumbnail below.
Please, keep in mind, I am not a healthcare professional and this should not be taken as medical advice. It is meant to show how a complicated issue, like contracting a respiratory virus has many causes, but by understanding those cause-and-effect relationships in a visual format, we’re able to evaluate possible solutions that would lower our risk of becoming infected. In addition, most of the cited research is based on the flu and other respiratory viruses, not COVID-19. Healthcare professionals, scientists and researchers are still working to understand the virus to make us all safer during the pandemic. For those working tirelessly, thank you.
This is the first blog in a series about understanding respiratory diseases and how we can mitigate the risk of contracting this deadly virus. By building a Cause Map diagram and citing evidence (in this case, scientific research studies), we can better understand a complex issue through the use of the visual diagram.
This is the second blog in a three blog series on reducing your risk of contracting the COVID-19 virus. See how the full Map of this complex issue during my upcoming webinar, "Reduce Your Risk of COVID-19 Infection: How a Cause Map™ Diagram Makes Sense of a Complex Issue" on April 8, 2020.
If you are interested in how using a Cause Map diagram can help you break down complex problems to find more effective solutions, check out one of our upcoming online workshops or online short courses.